
Finally, it should be noted that, even with a strict telephone triage protocol, diagnosis by telephone is only marginally better then random chance.

Women who had a previous diagnosis of vulvovaginal candidiasis were also inaccurate in their self-diagnosis, but they were more likely to self-treat. A recent questionnaire study 4 of 634 women found that only 11 percent were able to accurately recognize the classic case scenario for yeast infections. However, this number may represent an overestimate because patients in this study had been initially screened by telephone and were only evaluated and included in the study if they had symptoms consistent with vulvovaginal candidiasis. Initial data 3 suggested that women with a prior diagnosis of vulvovaginal candidiasis were able to make an accurate diagnosis up to 82 percent of the time based on symptoms alone. They were, therefore, using these medications inappropriately and, in at least the 15 percent of women in the study who had irritant dermatitis, their self-treatment played a role in the perpetuation of their symptoms.Įstimates of how accurately women are able to self-diagnose RVVC are difficult to obtain. Most of these women thought they had RVVC but, when they were evaluated at a specialty referral center, only 28 percent were diagnosed with RVVC. In one survey 2 of 105 women with chronic vaginal symptoms, 73 percent self-treated with OTC products and 42 percent used alternative medicines. Women are encouraged to self-medicate, and women with chronic vaginal symptoms often do. The purpose of this article is to summarize the current concepts in the evaluation of women with chronic vulvovaginal symptoms and to discuss recurrent vulvovaginal candidiasis (RVVC) in detail.ĭespite the extensive use of medications to treat vaginal symptoms, the appropriateness of their use is undermined by an attitude that deems an accurate diagnosis unnecessary. In conjunction with the establishment of these centers, studies of chronic vaginitis have been undertaken and new approaches to the problem have been investigated. In the past few decades, centers devoted to evaluating and treating women with chronic vaginitis have been established at various academic medical centers. Given that millions of women contract vaginitis, it is not surprising that a subpopulation of women with chronic vaginitis (defined here as some type of chronic vulvar or vaginal symptom lasting more than six months) exists. Over-the-counter (OTC) antifungal therapies now rank among the top 10 best-selling OTC products in the United States with an estimated $250 million in sales annually. Vaginitis accounts for more than an estimated 10 million physician office visits annually, and it remains the most common reason for patient visits to obstetrician-gynecologists.
Infections caused by other species of yeast may be more resistant to standard treatment approaches.įor any physician involved in the health care of women, the treatment of vaginitis remains a challenge. Long-term oral antifungal therapy will break the pattern of recurrence in many patients. In patients with RVVC caused by Candida albicans, host factors may play an important role.

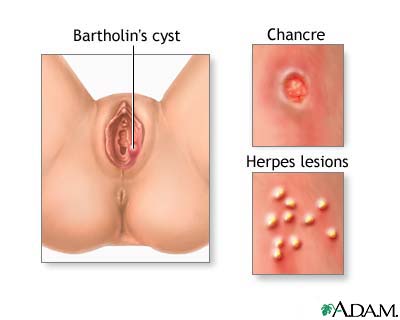
The most common causes of chronic vaginal symptoms are recurrent vulvovaginal candidiasis (RVVC), vulvar vestibulitis syndrome and irritant dermatitis. Fungal cultures are an important component of the work-up. Establishing a proper diagnosis will lay the foundation for an effective therapeutic plan. Frequently ignored by the medical community, chronic vulvovaginal symptoms are relatively common and can be frustrating for patients and physicians.


 0 kommentar(er)
0 kommentar(er)
